Lower Back Bedsores & Elder Neglect in New Jersey
For residents in nursing homes or long-term care facilities, sacral pressure ulcers are among the most serious—and preventable—signs of neglect. These wounds develop on the lower back near the tailbone, a high-risk area for those who are confined to beds or wheelchairs. What may begin as a small red spot can escalate quickly into a deep, infected wound involving muscle, tissue, and bone. When that happens, the consequences aren’t just physical—they’re legal. At the Law Office of Andrew A. Ballerini, we’ve seen firsthand how these injuries result from lapses in basic care like repositioning, hygiene, and wound monitoring. Families deserve to understand how these ulcers form, when they cross the line into nursing home neglect, and what rights they have under New Jersey law. If you believe your loved one may have suffered due to improper care, contact us to schedule a free consultation.
Key Takeaways
- Sacral pressure ulcers are among the most severe types of bedsores and often signal neglect in nursing homes.
- These injuries can progress quickly from skin irritation to deep wounds involving muscle and bone.
- Proper repositioning, hygiene, and nutrition are essential to prevent sacral ulcers in immobile residents.
- When facilities fail to follow care protocols, the resulting harm may justify legal action under New Jersey law.
- Families should document the injury, request medical records, and consult a nursing home abuse attorney as soon as possible.
Why the Sacral Region is So Vulnerable
The sacrum, located at the base of the spine near the tailbone, is one of the most pressure-prone areas on the human body—especially for elderly individuals with limited mobility. When a resident spends extended time in one position, such as lying in bed or sitting in a wheelchair, constant pressure on the sacrum can restrict blood flow and begin to damage tissue. Over time, this pressure leads to skin breakdown and eventually open wounds known as pressure ulcers. Without early intervention, what starts as mild irritation can rapidly become a deep wound involving fat, muscle, and even bone.
In long-term care settings, this area requires routine monitoring, proper hygiene, and frequent repositioning to avoid tissue damage. Facilities must follow specific protocols to minimize risk, including pressure relief schedules, use of therapeutic mattresses, and skin assessments. When these steps are skipped—whether due to staff shortages or poor training—residents face preventable harm. We frequently see this pattern in bedsores and pressure ulcer cases involving neglect.
If you suspect that your loved one has developed a sacral wound due to lack of care, document the injury and speak to a qualified nursing home abuse attorney about your options. Early legal guidance can help preserve evidence and protect your family’s rights.
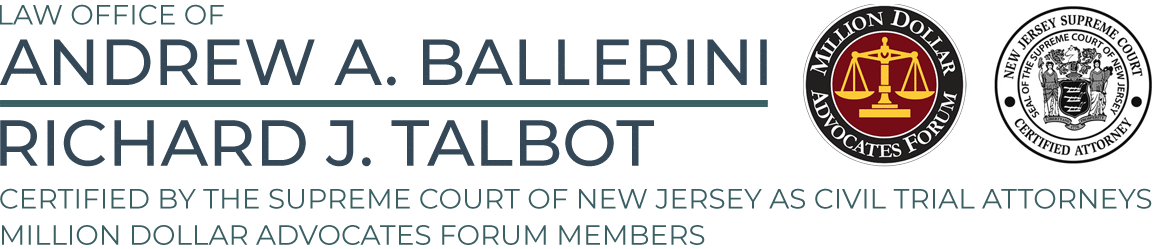
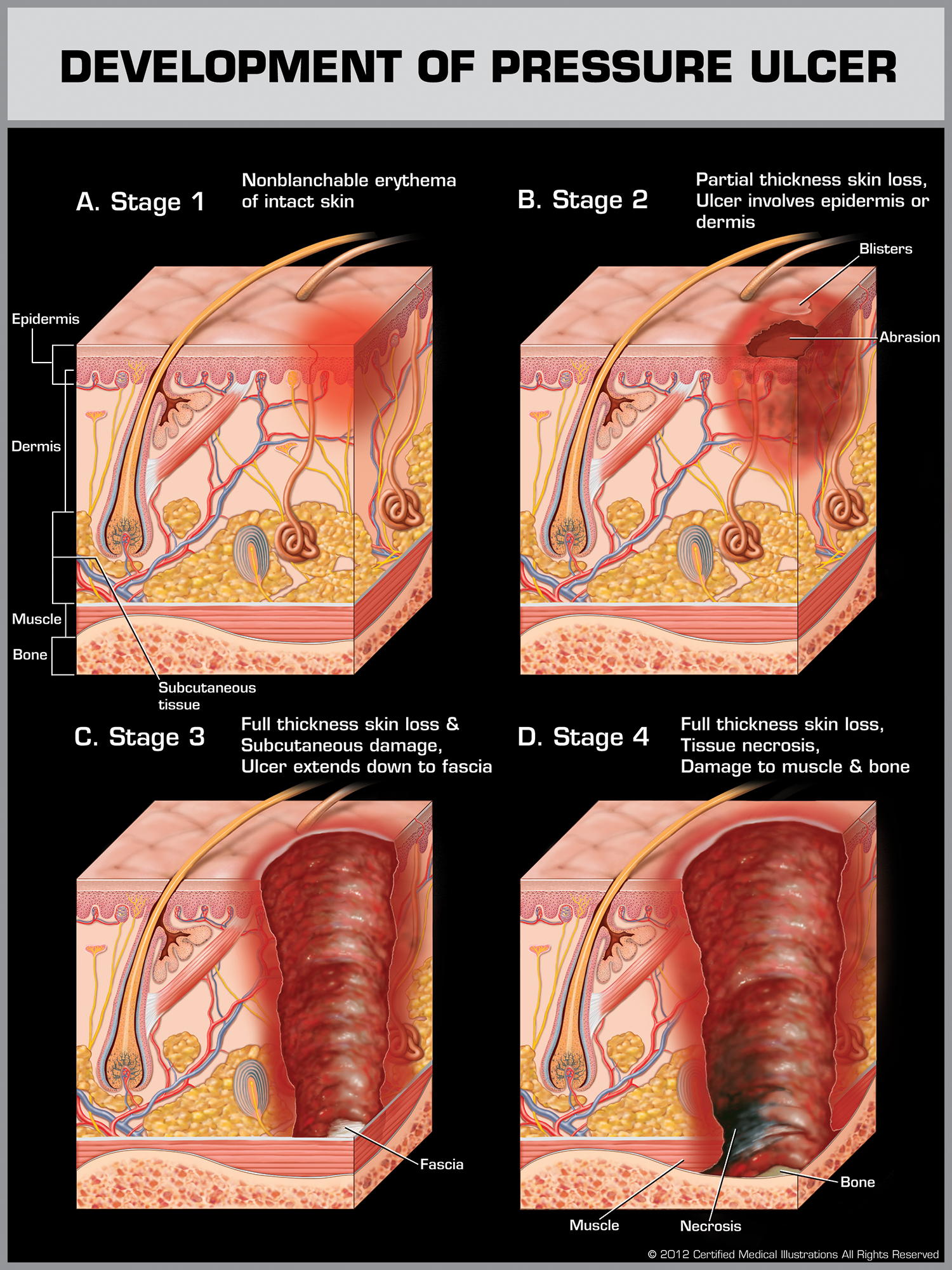
Understanding the Four Stages of Sacral Pressure Ulcers
Clinically, sacral pressure ulcers are classified into four stages based on the depth and severity of the tissue damage. Each stage indicates how far the wound has progressed—and how urgent proper medical intervention has become. Recognizing the signs early can make the difference between a treatable condition and one that leads to lasting harm.
Stage 1: Nonblanchable Redness
At this stage, the skin over the sacrum appears red or discolored but remains intact. The area may feel warm or firm to the touch, and the redness won’t fade when lightly pressed—a condition known as nonblanchable erythema. While no open wound exists yet, this is a clear early warning sign.
Stage 2: Partial-Thickness Skin Loss
The skin begins to break open, often appearing as a shallow ulcer or blister. The top layer (epidermis) and possibly part of the underlying dermis are damaged. This stage is often painful and especially vulnerable to infection. Families should request immediate wound care documentation and photographic records.
Stage 3: Full-Thickness Tissue Loss
By Stage 3, the ulcer extends below the skin and into the fat layer. Slough (a yellowish tissue) may be present, and the wound often forms a deep crater. At this point, a specialized wound care plan is required. Facilities should be using pressure-relieving mattresses and performing frequent repositioning.
- Daily skin assessments by trained staff
- Documented wound care protocols
- Family communication logs showing care plan updates
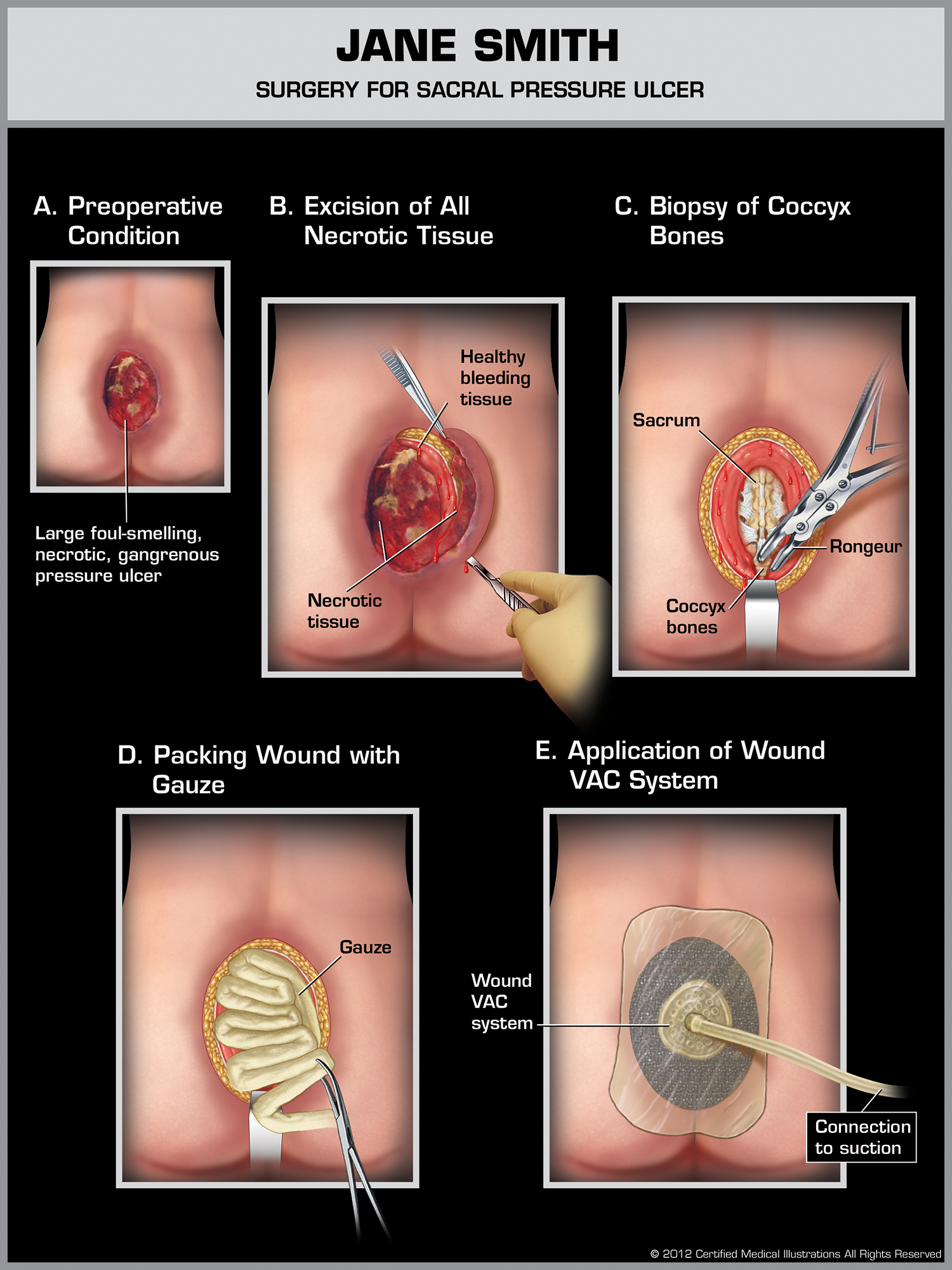
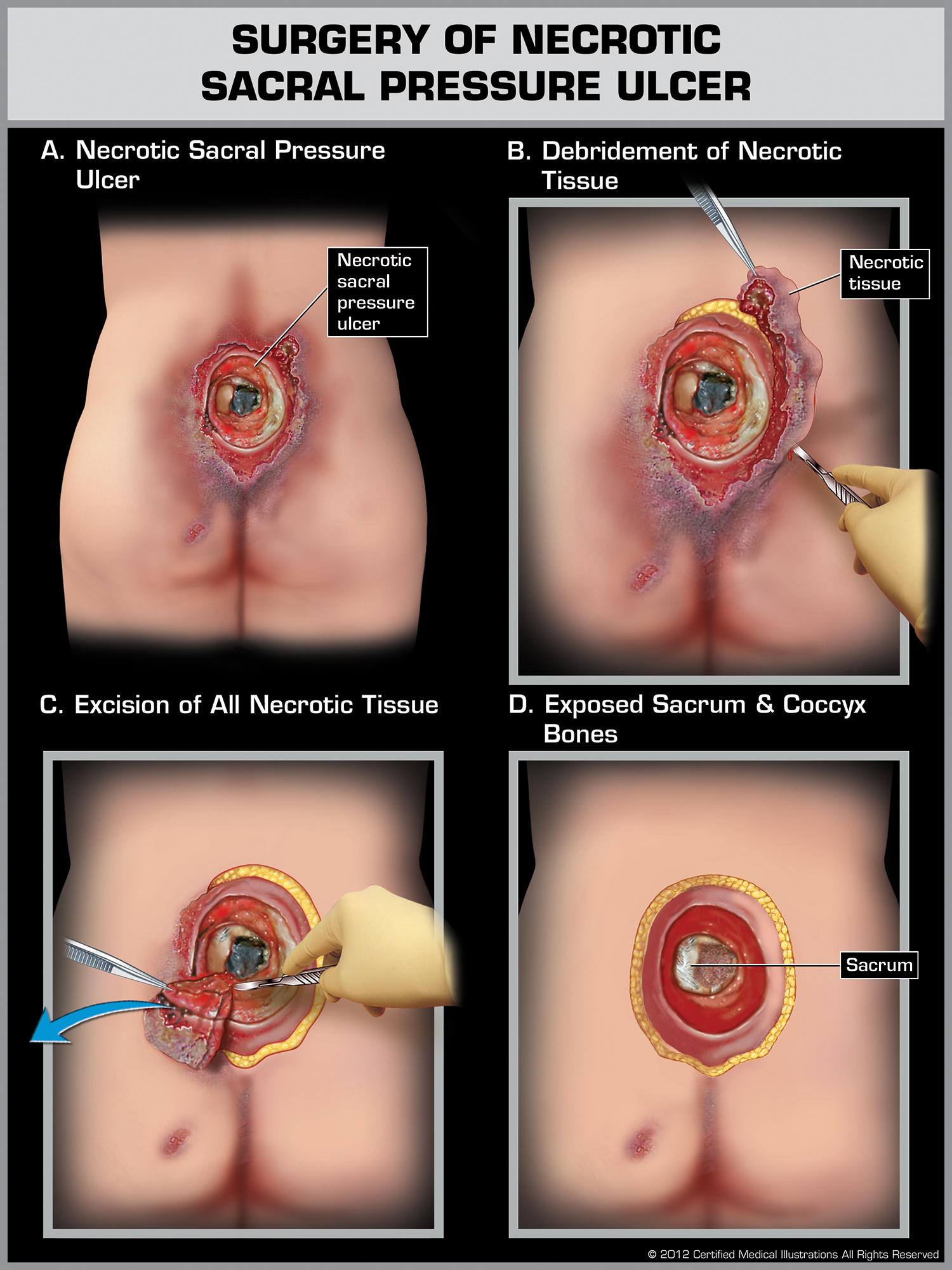
Stage 4: Extensive Tissue Damage
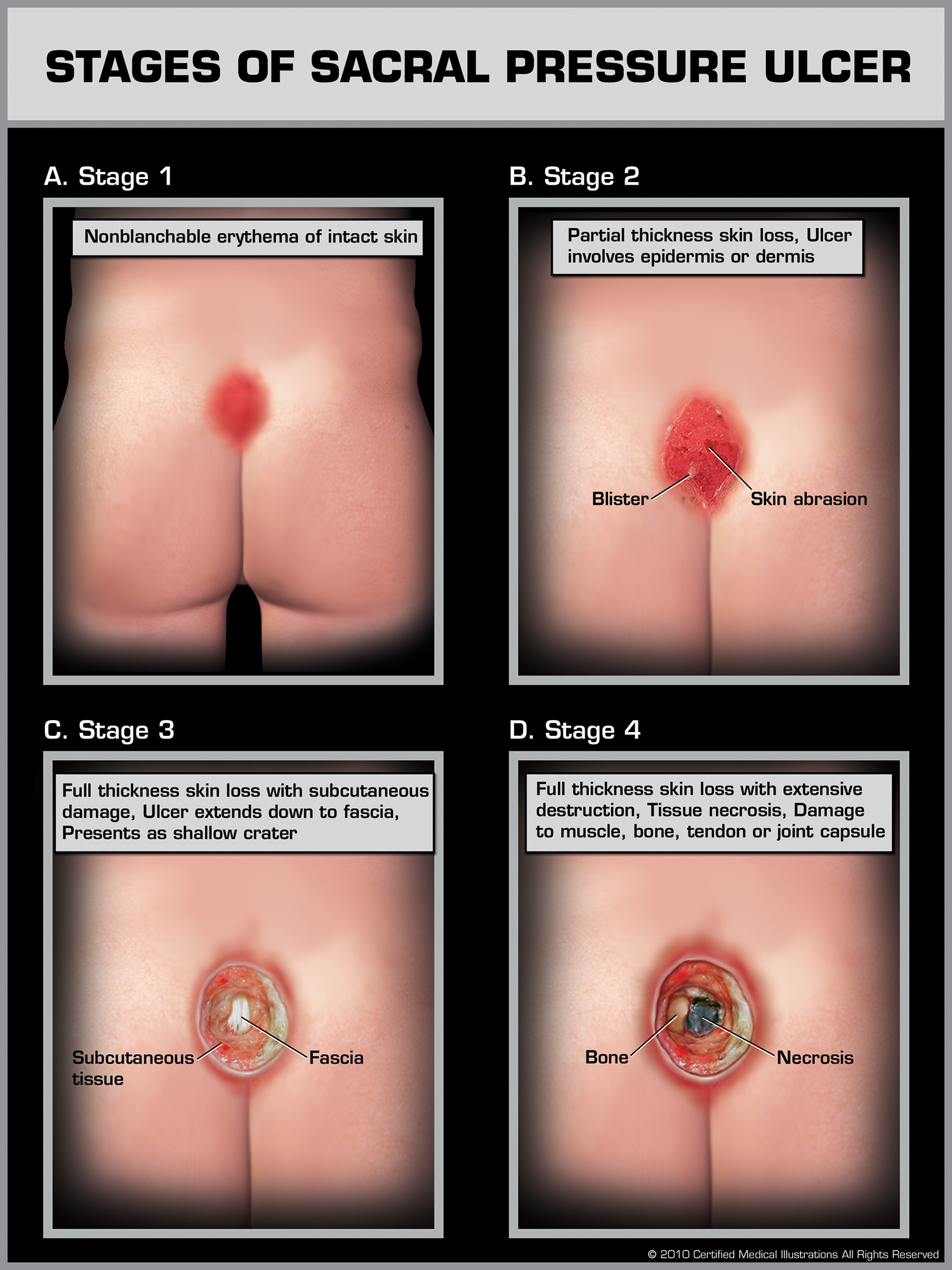
This is the most severe form of pressure ulcer, involving full-thickness skin loss with exposure of muscle, tendon, or even bone. Necrotic tissue (eschar or slough) may be present. These wounds often require surgical debridement and long-term care. They are also the most likely to involve serious complications such as sepsis.
Families should seek immediate legal guidance if a wound reaches Stage 4, particularly if there is no documentation of prior stages. These injuries typically result from long-term neglect or failure to follow required care standards. If you’re facing a situation like this, our team can help. Learn more about what qualifies as nursing home neglect and how it may apply to your case.
How These Wounds Progress Beneath the Surface
Not all pressure ulcers look serious at first glance. In fact, some of the most dangerous wounds begin beneath the skin, where damage develops out of sight. This is especially true in the sacral region, where prolonged pressure can cause deep tissue injury before any surface symptoms appear. Families often notice a dark or bruised area on the lower back—what looks minor may already involve damaged muscle or fat.
Why Surface Appearance Can Be Misleading
A sacral bedsore doesn’t have to be open to be dangerous. *Deep Tissue Injuries (DTIs)* occur when pressure or shear forces cause damage below the skin before it becomes visible. The area may feel firm, boggy, or warmer than surrounding tissue. If left unaddressed, the damage can evolve rapidly into a Stage 3 or Stage 4 ulcer.
What Speeds Up Bedsore Progression
Several factors can cause sacral wounds to worsen quickly—sometimes within hours. These include:
- Unrelieved pressure over bony areas like the tailbone
- Shear from dragging the body across bedding
- Excess moisture from incontinence or poor hygiene
- Compromised nutrition or dehydration
When a resident is not repositioned, cleaned, or nourished appropriately, tissue damage accelerates. You can learn more about how basic needs like hygiene and hydration impact skin health on our malnutrition and dehydration page.
Why Early Action Matters
Early-stage bedsores can often heal with non-invasive care and proper pressure relief. But when sacral ulcers go untreated, they become deeper, more painful, and significantly harder to reverse. By the time the wound is visible at Stage 3 or Stage 4, surgical intervention may be the only option—and the damage may already qualify as medical neglect.
If a facility fails to identify and treat pressure injuries early, that’s a red flag. Medical records, wound care notes, and communication logs often reveal whether a nursing home followed the required care protocols. We can help you review this documentation and determine whether a legal claim is appropriate.
What Sacral Pressure Ulcers Can Reveal About Nursing Home Neglect
Not all pressure ulcers are the result of unavoidable health decline. In many cases, especially those involving sacral wounds, the injuries stem from facility-wide failures to follow basic care standards. These include lapses in monitoring, delayed treatment, insufficient staffing, or failure to follow an individualized care plan. When these protocols break down, the result is often more than just a medical problem—it becomes a matter of legal accountability.
Neglect Is Often a Pattern—Not a One-Time Mistake
We regularly see pressure ulcer cases where a facility has failed in several key areas. Common patterns include:
- Inadequate repositioning: Residents are left in the same position for hours at a time.
- Incomplete documentation: Wound care records are missing, inconsistent, or falsified.
- Delayed escalation: Early signs of tissue breakdown are ignored or downplayed.
- Low staffing levels: Care teams are overworked and unable to maintain proper protocols.
These failures are not isolated errors—they reflect a systemic issue in how the facility operates. And under New Jersey law, this may constitute nursing home neglect. Learn more about what qualifies as neglect under state regulations by visiting our page on New Jersey nursing home neglect.
Signs Families Should Not Ignore
If you’re concerned about how your loved one developed a sacral ulcer, look for other warning signs that neglect may be involved:
- Worsening wounds with no explanation or treatment updates
- Staff refusing to share care plans or wound progression notes
- Sudden weight loss, dehydration, or repeated infections
- Lack of communication from facility leadership or nurses
These red flags often accompany serious underlying problems in care delivery. If you’re unsure whether neglect is occurring, our team can help review your case. You can also read more about related risks such as malnutrition and hygiene-related injuries, which often accompany advanced pressure wounds.
Legal Options for Families in New Jersey
When a preventable pressure ulcer leads to serious harm, families have the right to pursue accountability. New Jersey law protects nursing home residents from neglect and abuse, and facilities are held to specific standards of care. When those standards are not met—and a sacral pressure ulcer develops as a result—legal action may be appropriate.
When Is a Lawsuit Justified?
A legal case may be justified if medical records or firsthand evidence show that:
- The facility failed to reposition the resident at required intervals
- No wound care plan or risk assessment was documented
- The ulcer progressed through multiple stages without intervention
- Staff ignored early signs of skin breakdown or infection
Even if a facility blames the resident’s condition, the presence of a Stage 3 or Stage 4 sacral ulcer may indicate that proper care was not provided. These injuries are often signs of ongoing neglect—not sudden decline.
How Our Firm Can Help
At the Law Office of Andrew A. Ballerini, we focus on helping families hold negligent nursing homes accountable. Our team, led by attorney Richard J. Talbot, has extensive experience handling complex bedsore and elder neglect cases across New Jersey. We review wound care records, care plans, staff logs, and photographic evidence to determine whether legal action is appropriate.
We offer free consultations and work on a contingency basis—meaning you don’t pay unless we secure compensation for your family. Whether the injury involves a severe ulcer, wrongful death, or systemic neglect, we’re here to help guide you through the legal process.
Take the First Step
If you believe your loved one developed a sacral pressure ulcer due to nursing home neglect, don’t wait. Time-sensitive records and evidence may be critical to your case. Contact our team today to schedule a consultation. We can meet at our Cherry Hill office, in your home, or virtually—whatever works best for your family.
You can also review past results on our case results page to see how we’ve helped other families pursue justice.