Heel Pressure Ulcers in Nursing Homes: A Preventable Tragedy
When the Smallest Wound Reveals the Deepest Neglect
You placed your loved one in a New Jersey nursing home for safety and support. But now you’re facing something you never expected – a painful bedsore on their heel that just won’t heal. Maybe it started as a red spot, barely noticeable. Now it’s a deep wound, and no one can give you a straight answer about how it happened. If you’re feeling grief, anger, or confusion, you’re not alone. At the Law Office of Andrew A. Ballerini, we’ve seen firsthand how heel pressure ulcers often signal deeper issues – like chronic understaffing, poor training, or outright neglect. And we believe one thing above all: bedsores don’t have to happen.
Heel ulcers often develop when care protocols break down – when immobile residents aren’t turned, when staff miss early warning signs, or when facilities fail to provide even the most basic protections. These wounds progress through well-documented stages, and the signs are often visible well before they become life-threatening. Under New Jersey elder care laws, families have the right to demand answers, access records, and take legal action when facilities fail to uphold their duty of care.
Key Takeaways
- Heel pressure ulcers are preventable injuries, not an inevitable part of aging.
- They often develop when immobile residents are not properly turned or monitored.
- The heel is a high-risk site due to limited padding and poor circulation in elderly patients.
- Warning signs include redness, swelling, open wounds, or dressing changes without explanation.
- Federal and New Jersey care standards require daily skin checks, repositioning, and proper wound care.
- Stage 3, Stage 4, or infected heel ulcers may indicate serious neglect or even wrongful death.
- Families have the right to request documentation and pursue legal action when care falls short.
What Are Heel Pressure Ulcers?
Understanding Pressure Sores on the Heels
Heel pressure ulcers – also known as pressure sores or bedsores – are injuries that develop when prolonged pressure cuts off circulation to the skin and underlying tissue. In nursing homes, they’re most commonly found on residents who are immobile, bedbound, or unable to reposition themselves without assistance. The heel is one of the most vulnerable areas because it has thin skin, limited fat padding, and often rests directly against a mattress or footboard for long periods.
Why the Heel is So Vulnerable
The anatomy of the heel makes it a high-risk zone for pressure injuries. There’s very little cushioning between the heel bone and the skin, which means even a few hours of unrelieved pressure can begin to damage tissue. Circulation is already compromised in many elderly residents – especially those with diabetes, peripheral artery disease, or limited mobility – making it even harder for the body to heal. When a facility fails to provide proper offloading devices, heel protectors, or routine skin checks, pressure sores can appear quickly and worsen fast.
Who’s Most at Risk?
Not every resident is equally at risk. Pressure sores on the heels are more likely to occur in individuals with:
- Limited mobility or those confined to a bed or wheelchair
- Chronic conditions like diabetes or vascular disease
- Malnutrition or dehydration, which weakens the skin
- Sensory impairments, making it hard to feel pain or pressure
- Incontinence, which increases skin moisture and infection risk
For these residents, prevention isn’t optional – it’s a medical necessity. When it’s ignored, the result isn’t just a wound. It’s a sign that someone wasn’t doing their job.
How Heel Ulcers Develop in Nursing Homes
The Slow Breakdown That Should Have Been Prevented
Heel pressure ulcers don’t appear overnight. They develop slowly – sometimes silently – when the basic routines of care are overlooked. For residents who can’t move on their own, just a few hours in the same position can start to damage tissue. Without regular repositioning, offloading devices, or proper skin inspections, pressure begins to cut off circulation. Once that happens, the skin weakens, tissue dies, and an ulcer forms. What starts as mild redness can escalate into a deep, infected wound in a matter of days.
Breakdowns in Routine Care
Most heel ulcers are entirely preventable with standard protocols. Nursing home staff are trained to:
- Reposition immobile residents at least every two hours
- Use heel cushions, boots, or floating devices to relieve pressure
- Perform daily skin checks, especially on high-risk areas
- Adjust care plans based on risk factors like diabetes or past ulcers
When these steps aren’t followed—or when a facility is understaffed – wounds are missed, care is delayed, and injuries deepen. That’s when what should be a routine part of care becomes a serious health risk.
When Staffing Levels Matter
One of the most common causes of pressure ulcers is inadequate staffing. Even well-meaning caregivers can’t meet basic standards when they’re stretched too thin. We’ve seen this pattern again and again: fewer aides on the floor, longer times between rounds, and residents left in one position far too long. The result? More pressure injuries, more hospitalizations – and more preventable harm.
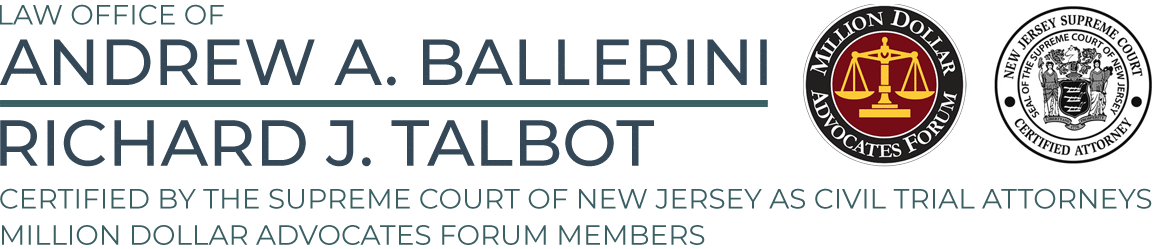
The Clinical Stages of Heel Pressure Ulcers
From Redness to Deep Wounds: What Each Stage Means
Understanding the stages of pressure ulcers is critical for recognizing when something is wrong – and how far it’s gone. The National Pressure Injury Advisory Panel defines these stages to guide both diagnosis and treatment. In many cases, families only learn about the injury when it’s already progressed to Stage 3 or 4. By then, the damage can be permanent or even life-threatening.
Stage 1: A Warning Sign
At this stage, the skin remains intact but shows signs of irritation – typically redness that doesn’t fade when pressed. It may feel warmer, firmer, or more painful than surrounding skin. This is the body’s first warning. If staff don’t take immediate action to relieve pressure, progression is likely.
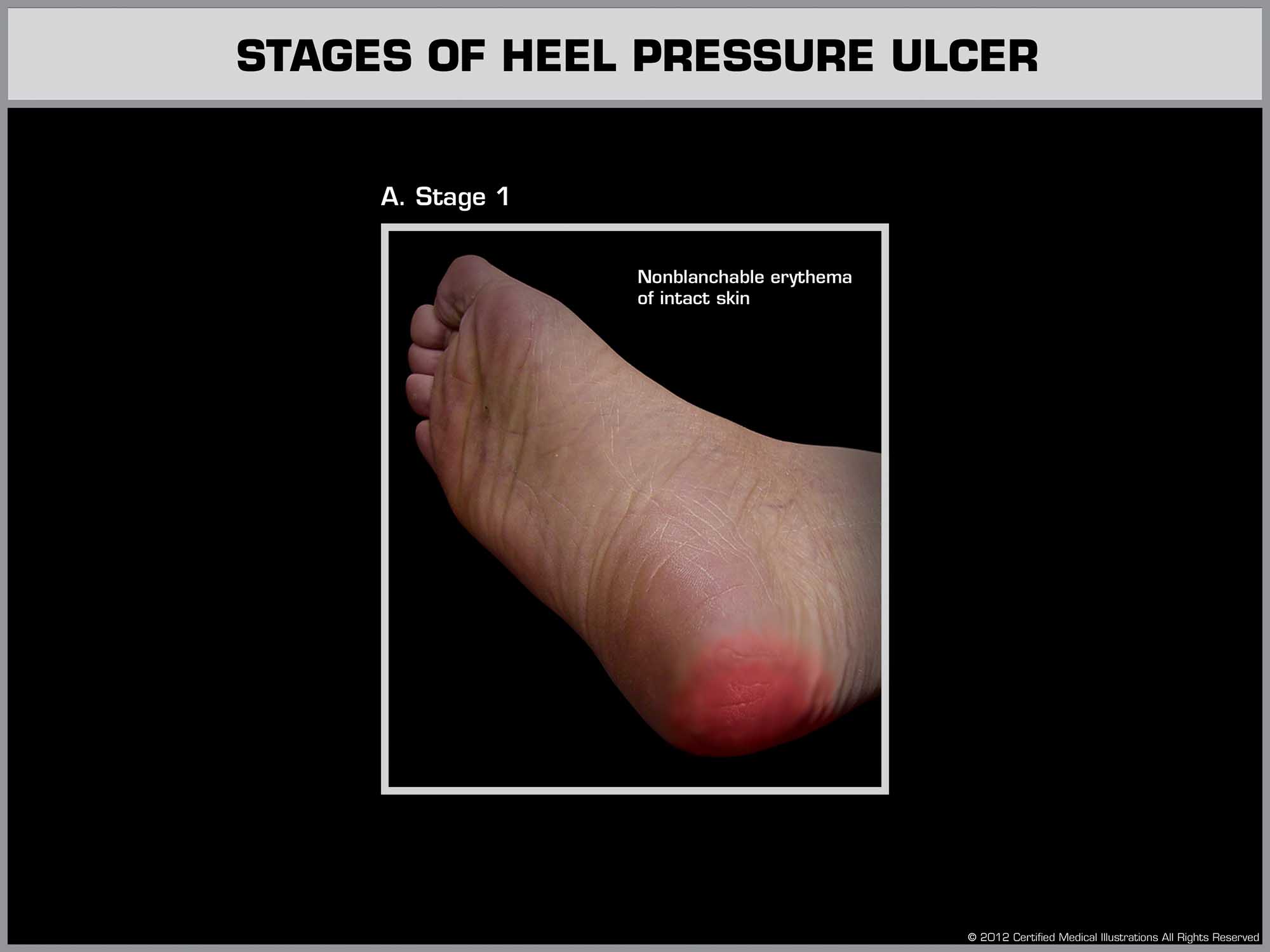
Stage 2: Skin Breaks Open
The top layer of skin breaks, forming a shallow wound that may look like a blister, scrape, or abrasion. It’s painful and vulnerable to infection. By Stage 2, clear documentation and an updated care plan should already be in place. If not, it’s a red flag.
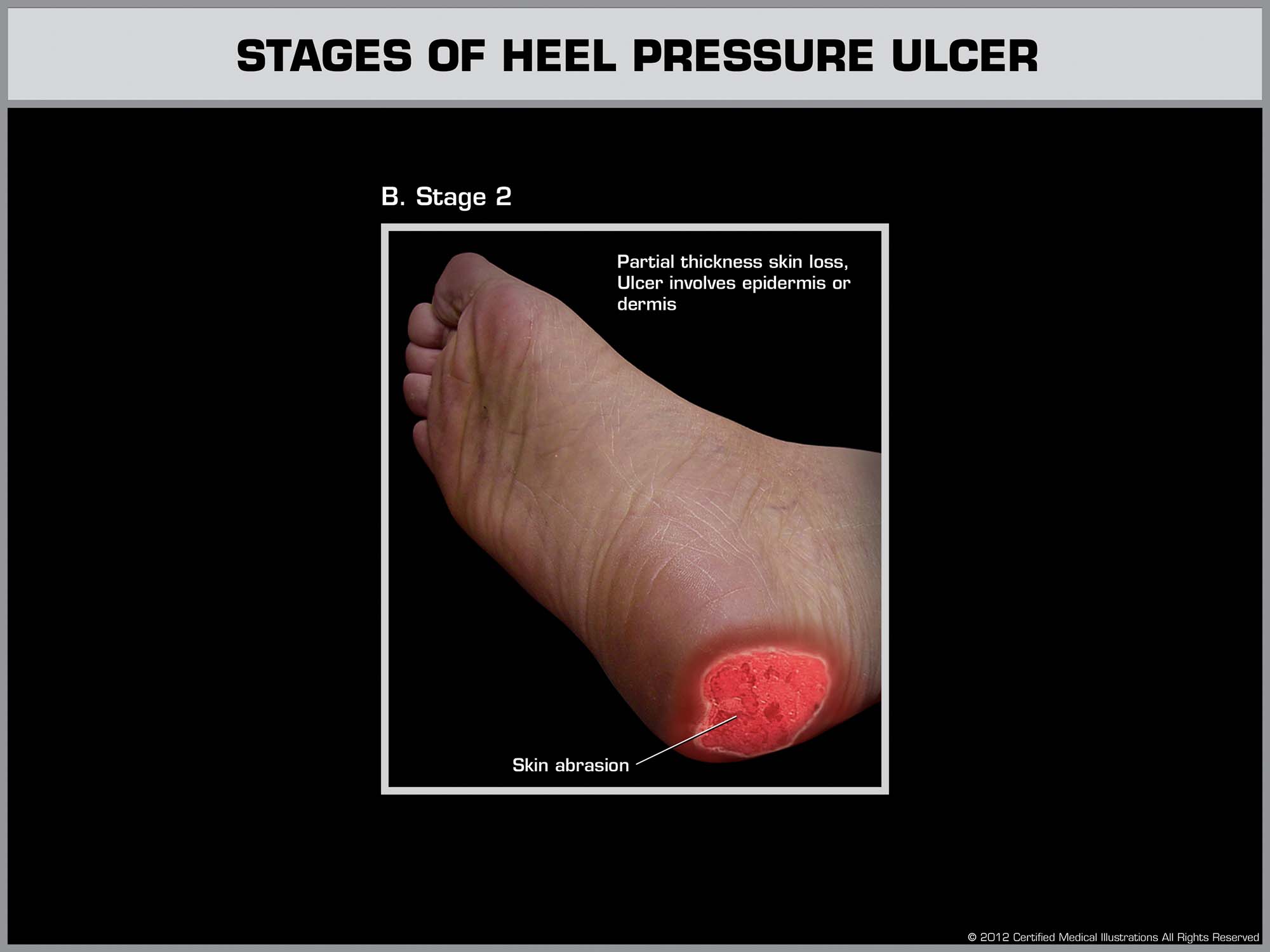
Stage 3: Damage to the Fat Layer
At Stage 3, the ulcer extends into the fat beneath the skin. The wound may appear as a deep crater, with signs of dead tissue or infection. This level of injury is serious and requires aggressive wound care – often involving specialists, debridement, and possibly surgery.
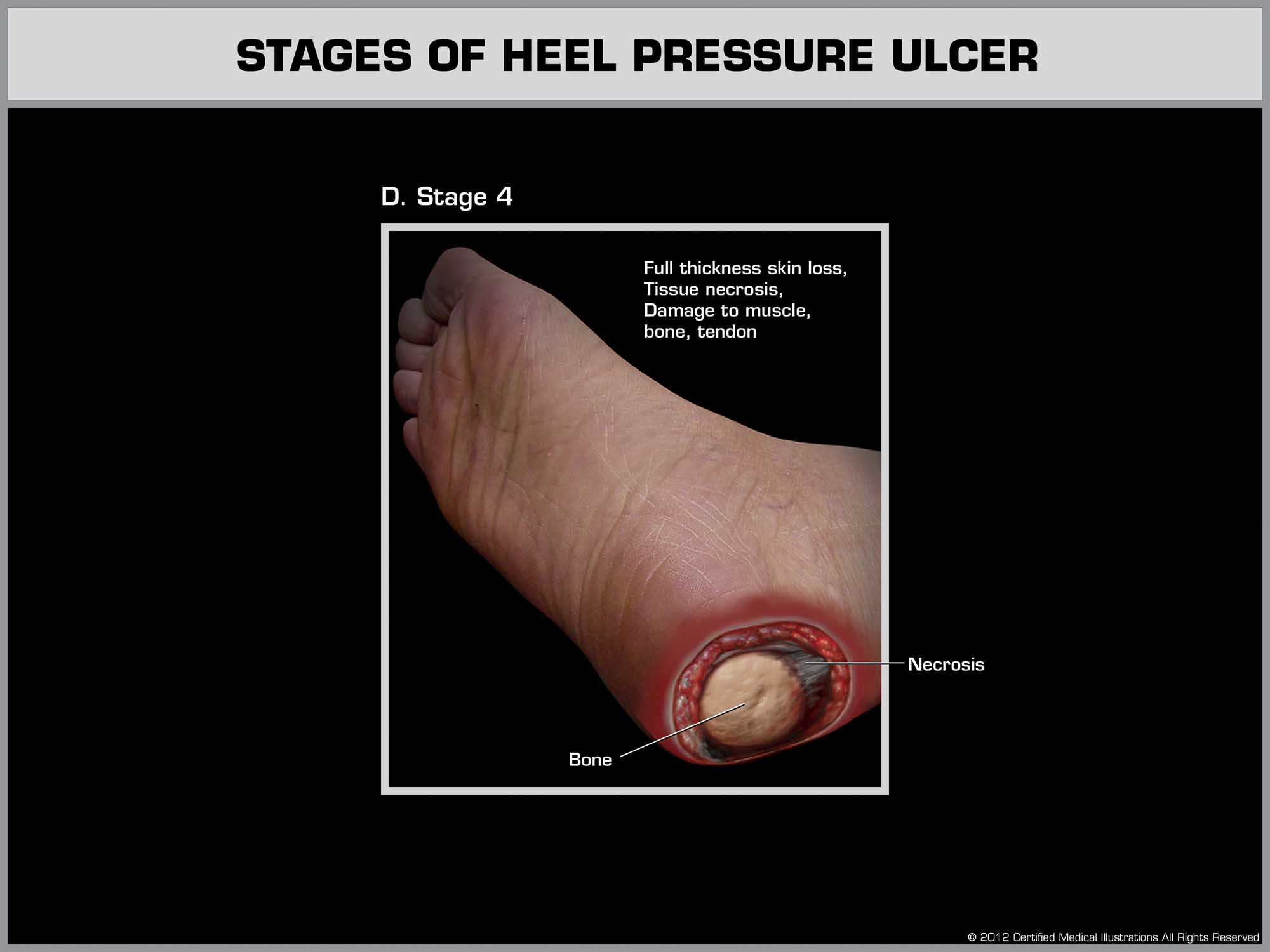
Stage 4: Exposure of Bone or Tendon
This is the most severe stage. The ulcer exposes muscle, tendon, or bone, increasing the risk of sepsis, osteomyelitis, or amputation. Stage 4 wounds are rarely the result of a one-time oversight. They typically reflect a long-term pattern of neglect or failure to monitor.
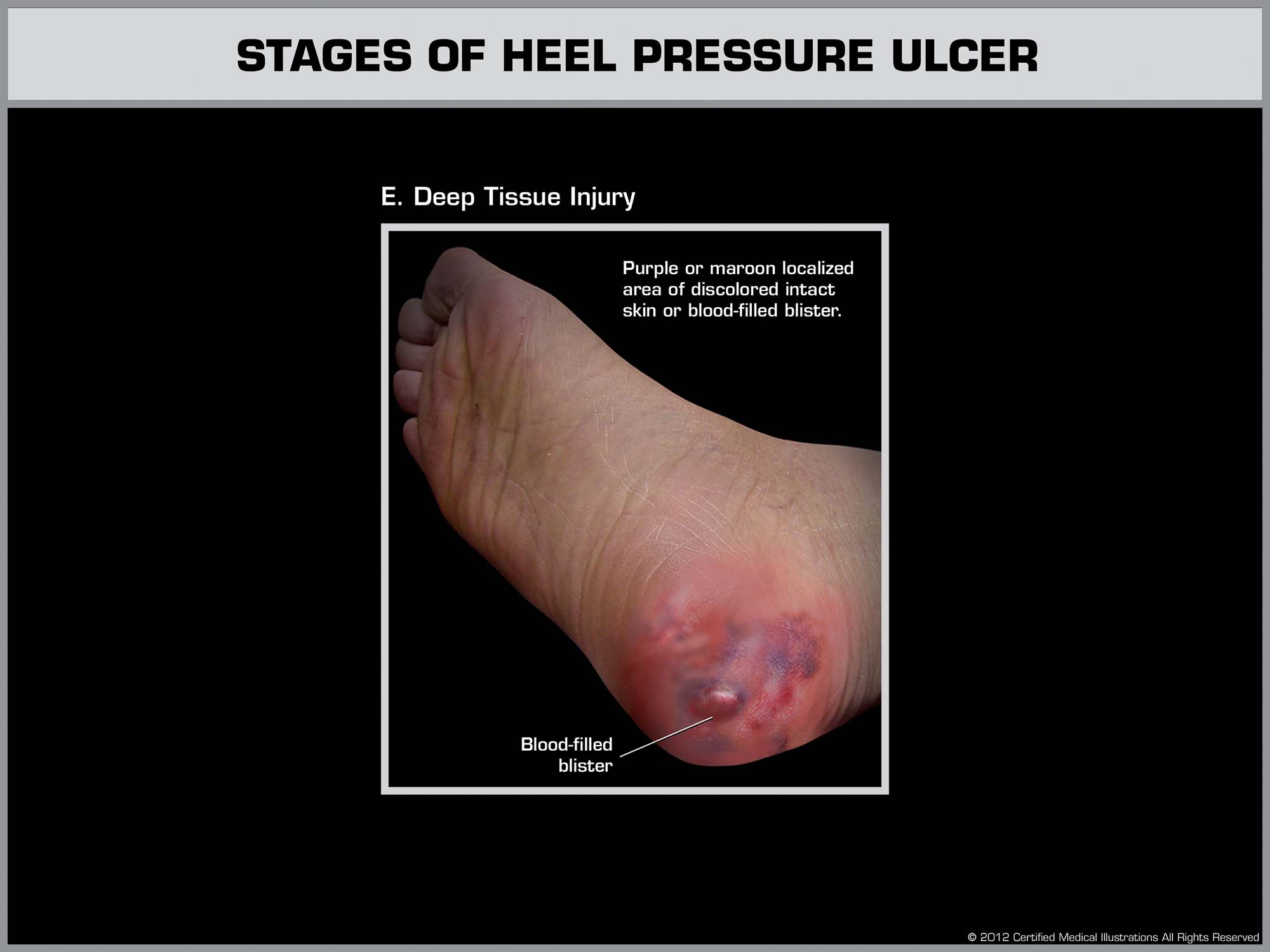
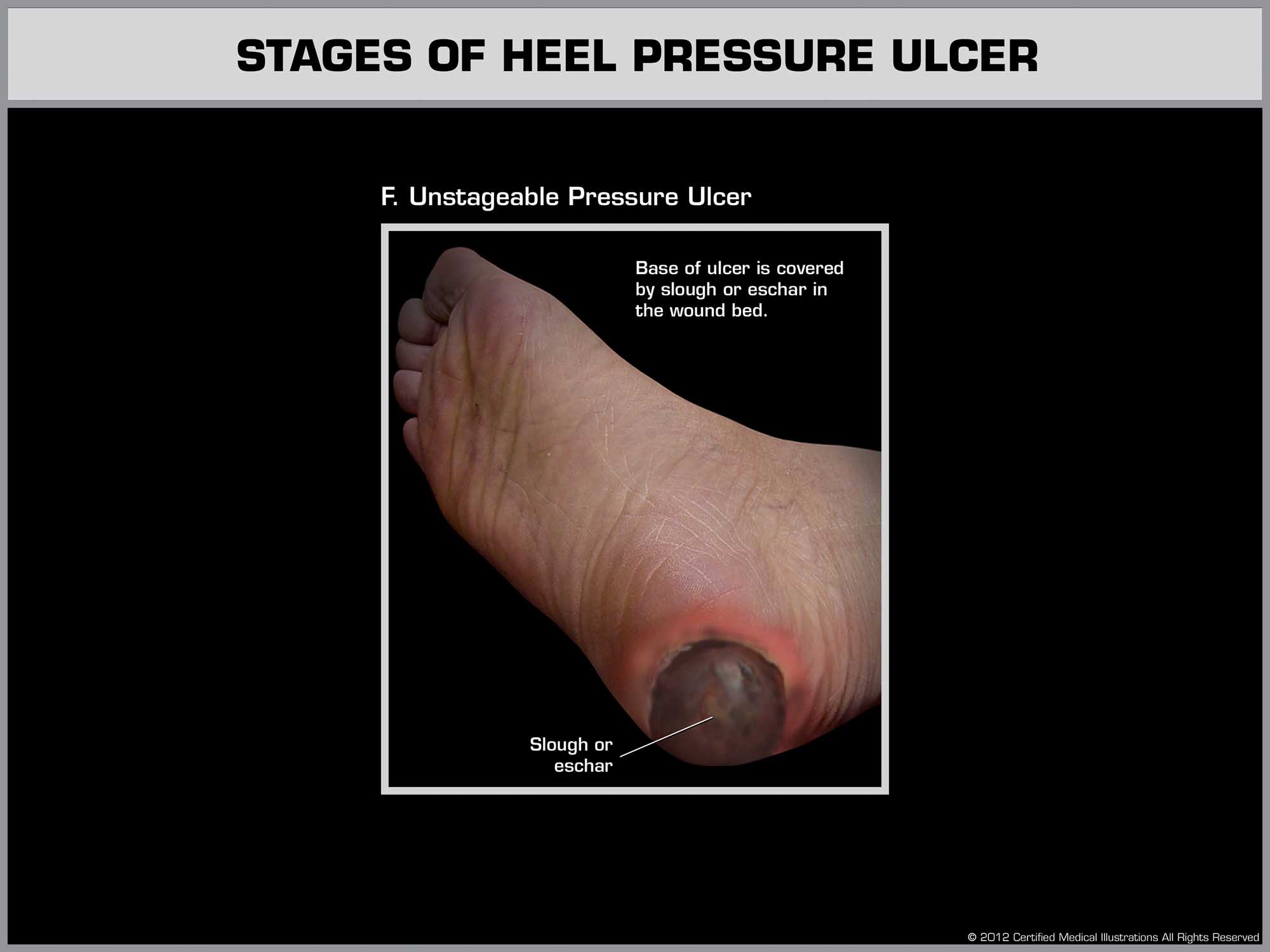
Unstageable or Suspected Deep Tissue Injury
Some heel ulcers are considered unstageable due to dead tissue covering the wound. Others fall under “suspected deep tissue injury” – when the skin appears bruised or discolored but the depth isn’t visible yet. Both require immediate clinical evaluation and aggressive intervention.
If your loved one developed a Stage 3, Stage 4, or unstageable heel ulcer, it’s not just a medical issue – it’s a legal one. These wounds don’t happen in well-run facilities that follow basic protocols. They happen when no one is watching.
Early Warning Signs Families Should Watch For
Don’t Wait Until It’s Too Late
Families are often the first line of defense. If you’re visiting your loved one in a New Jersey nursing home, pay attention to the little things – because pressure ulcers rarely start out looking serious. The earlier a heel bedsore is identified, the greater the chance of full recovery. When staff miss – or ignore – these warning signs, the results can be devastating.
What to Look For During Visits
You don’t need medical training to spot signs of trouble. Trust your instincts, and watch for:
- Redness or darkened skin on the heels that doesn’t fade when touched
- Swelling, warmth, or hardness in the heel area
- Blisters, open wounds, or drainage on socks or bedding
- Bandages or dressings that weren’t there before – with no explanation
- Complaints of heel pain, especially when being moved or touched
What to Ask the Staff
If you notice anything unusual, ask direct questions. You have the right to know:
- When was the wound first noticed, and how has it changed?
- Has a wound care nurse or physician examined it?
- Is there a written care plan for prevention and treatment?
- How often is your loved one being repositioned or offloaded?
Vague answers, inconsistent records, or delayed responses may point to deeper problems. Pressure ulcers don’t get better with silence—they get worse.
Standards of Care in New Jersey Nursing Homes
What Proper Care Should Look Like
Nursing homes in New Jersey are legally required to meet basic standards for resident care. That includes preventing pressure ulcers like those on the heel – especially in high-risk patients. The Centers for Medicare & Medicaid Services (CMS) and the New Jersey Department of Health both hold facilities accountable for failing to implement these protocols. If a bedsore develops, it often means something went wrong. If it worsens, it almost certainly did.
Key Prevention and Treatment Standards
Facilities must take proactive steps to reduce the risk of pressure injuries, including:
- Assessing skin integrity and risk factors upon admission and regularly thereafter
- Turning and repositioning residents at least every two hours, or more often if needed
- Using heel protectors, offloading boots, or floating heels to relieve pressure
- Providing adequate hydration, nutrition, and incontinence care
- Monitoring wounds daily and documenting all treatment steps
When Care Falls Short
A heel ulcer doesn’t happen in isolation – it’s usually part of a broader breakdown in care. Staff may be overworked, undertrained, or inattentive. Care plans may be outdated or ignored. And when facilities cut corners to save money, residents pay the price. The result is often a wound that’s allowed to deepen until infection, hospitalization, or even death occurs.
Facility Records Can Reveal the Truth
Families have the right to request documentation, including:
- Daily skin assessment logs
- Wound care notes and photographs
- Repositioning schedules
- Care plan updates and physician orders
If these records are missing, inconsistent, or contradictory, it may indicate neglect. No one should have to guess whether their loved one is receiving basic care.
When Heel Ulcers Signal Legal Neglect
Bedsores Don’t Have to Happen
Pressure ulcers – especially Stage 3, Stage 4, or infected wounds – are rarely just medical complications. In many cases, they’re the result of substandard care. When a nursing home fails to follow basic prevention protocols, delays treatment, or fails to notify family members about a wound, that’s not just poor care. It may be legal neglect.
How Neglect Often Shows Up
We’ve spoken with families who were told everything was fine – until their loved one was sent to the hospital with a life-threatening heel wound. Others discovered the injury only after death, when a funeral home or medical examiner raised concerns. These stories are heartbreaking. And they are far too common.
What to Document
If you suspect neglect, begin collecting information right away. You don’t need to confront staff directly, but you should request:
- Copies of the care plan and any wound care notes
- Records showing when the ulcer was first documented
- Photos or descriptions of the wound’s progression
- Names of staff assigned to your loved one’s care
If staff refuse to share this information, delay your request, or give conflicting answers, that may be a sign they’re trying to protect the facility – not the patient.
When to Speak With a New Jersey Nursing Home Attorney
If a heel ulcer led to hospitalization, amputation, or contributed to your loved one’s death, it’s time to ask hard questions. New Jersey law protects nursing home residents from neglect and abuse. Families have the right to investigate, access medical records, and pursue compensation when facilities fail in their duty of care.
An experienced nursing home neglect attorney can help you determine whether the injury was truly unavoidable – or whether it was caused by preventable failures. You don’t need to figure that out alone. We’re here to help.