Why Preventable Pressure Ulcers Happen
Far too often, families entrust the care of their loved ones to nursing homes—only to discover, sometimes too late, the telltale signs of neglect. One of the clearest and most painful indicators is the presence of bedsores, also known as pressure ulcers. These injuries don’t just appear overnight. They develop gradually, often due to lapses in basic care such as repositioning, monitoring, and attention to individual needs. Understanding how bedsores happen in nursing homes is crucial for families navigating the emotional and legal fallout of elder care failures. While some facilities may argue these wounds are an inevitable part of aging or illness, many are in fact preventable and stem from negligence, poor staffing, or systemic oversight. At The Law Office of Andrew A. Ballerini, we’ve seen firsthand how preventable injuries like these cause unnecessary suffering—and we’re here to help you hold negligent facilities accountable.
What Are Bedsores?
Understanding Pressure Ulcers and Why They Occur
Bedsores, also known as pressure ulcers or decubitus ulcers, are injuries to the skin and underlying tissue that develop due to prolonged pressure on specific areas of the body. These wounds are especially common in nursing home residents who are confined to beds or wheelchairs and unable to change positions without assistance.
Most commonly, bedsores form on bony areas such as the heels, hips, tailbone, and lower back. Without regular movement and attentive care, the pressure reduces blood flow to these regions, causing the skin and tissue to break down. If untreated, a mild sore can rapidly escalate into a deep wound that exposes muscle or bone—causing intense pain, infection, and in some cases, life-threatening complications.
Development of Pressure Ulcers/Bedsores
Clinically, bedsores—also known as pressure ulcers—are classified into four stages based on severity:
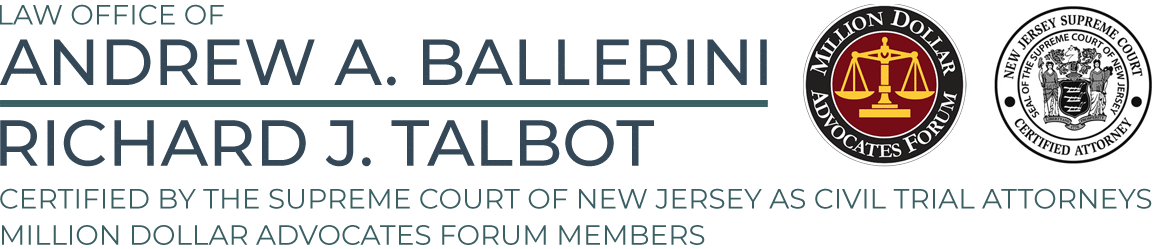
- Stage 1: Nonblanchable erythema of intact skin. The skin appears red and irritated but remains unbroken. It does not turn white (blanch) when pressed.
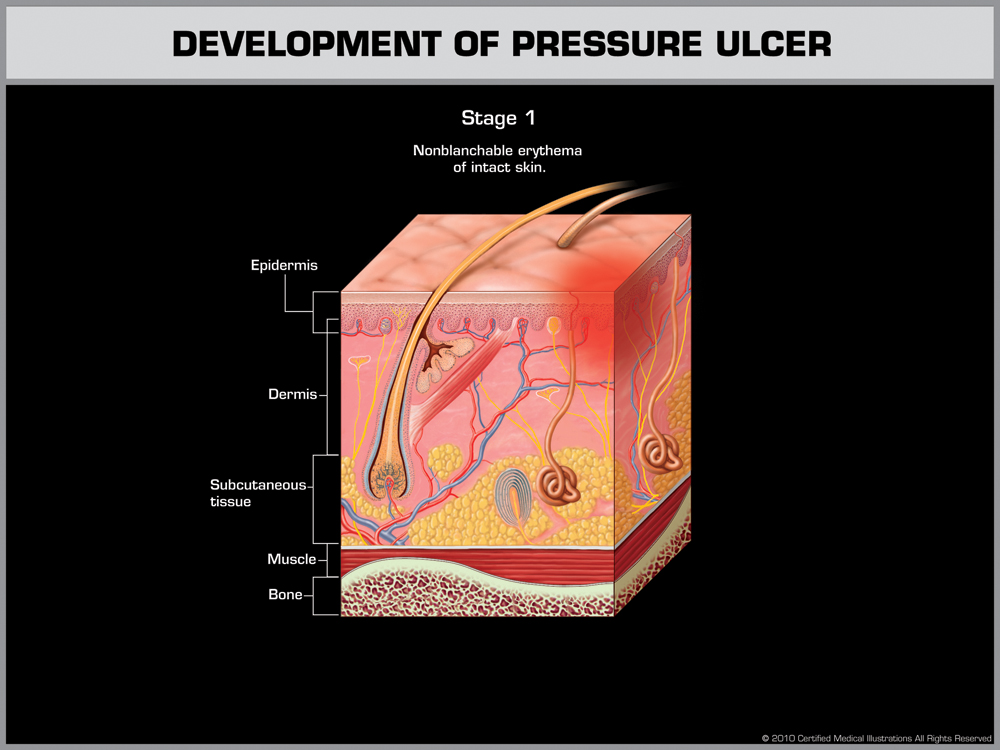
- Stage 2: Partial-thickness skin loss involving the epidermis or dermis. The wound may appear as a blister or shallow open sore with visible damage to the outer skin layer.
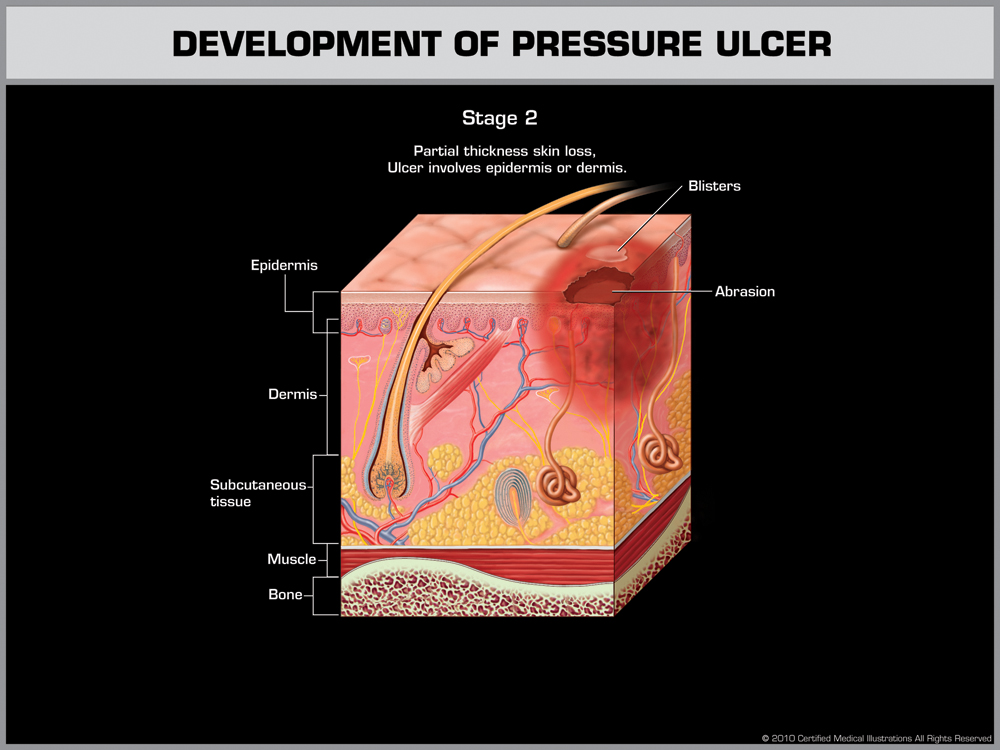
- Stage 3: Full-thickness skin loss with damage to subcutaneous tissue. The ulcer extends down to the fascia and appears as a deep wound, potentially exposing fat beneath the skin.
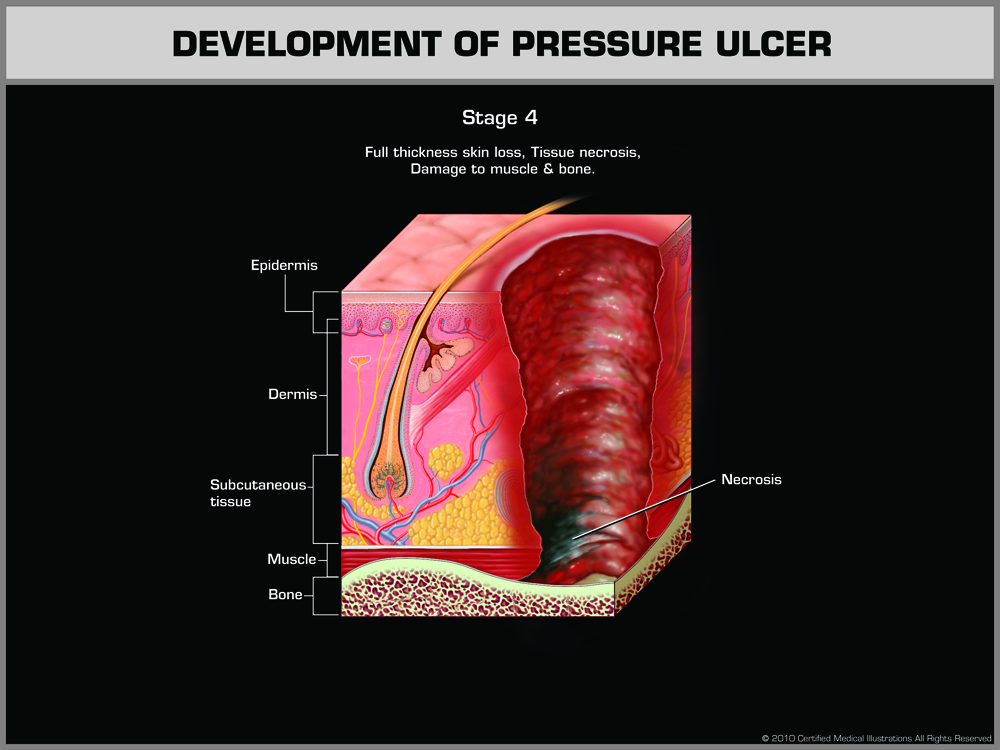
- Stage 4: Full-thickness tissue loss with extensive necrosis. Damage may involve muscle, tendon, or bone and is often accompanied by slough, eschar, or infection.
These injuries do not develop instantly—they result from sustained, unrelieved pressure over a period of time. Early detection and consistent preventative care are essential in any long-term care setting.
Additional Classifications
In addition to the four defined stages, two other types of pressure-related injuries are recognized by medical professionals.
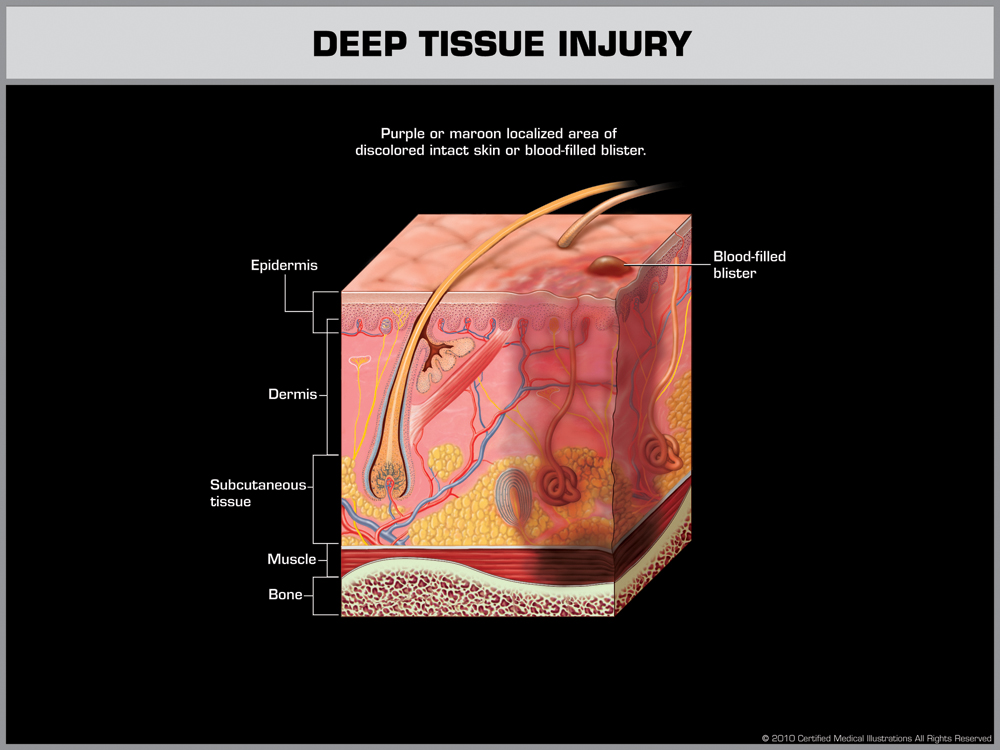
- Deep Tissue Injury (DTI): Deep Tissue Injury (DTI) – Appears as a purple or maroon area of discolored, intact skin or a blood-filled blister. Indicates damage beneath the surface before the skin breaks open.
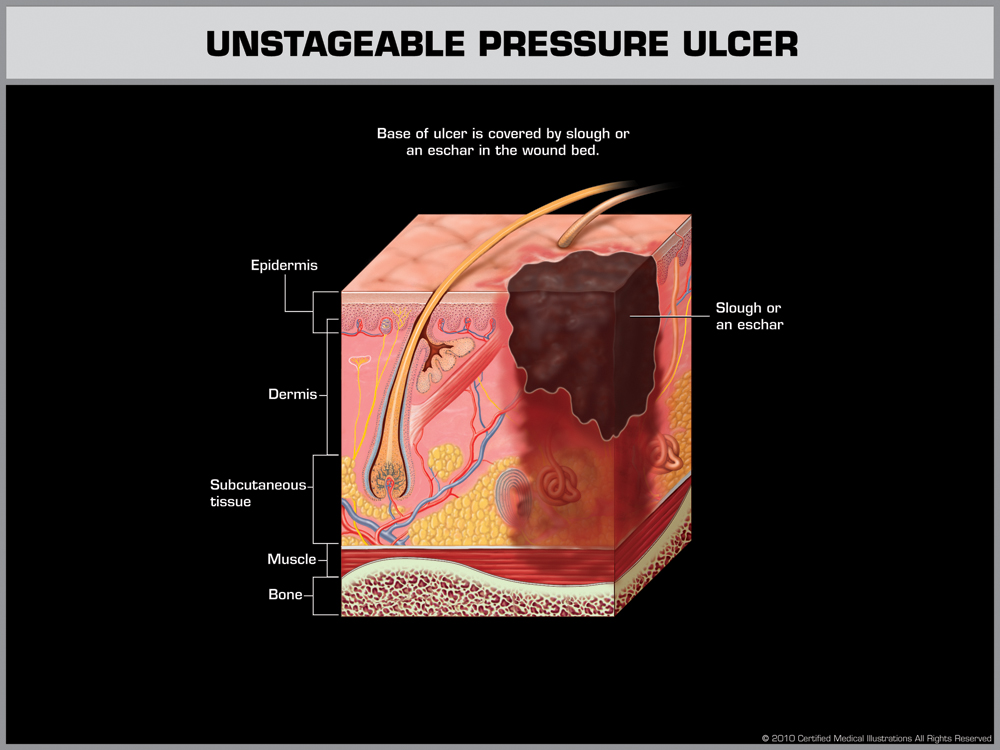
- Unstageable Pressure Ulcer: Full-thickness skin and tissue loss where the wound bed is covered by slough or eschar (dead tissue), preventing accurate staging until it is debrided.
They are classified separately because the extent of tissue damage cannot be fully determined on initial examination.
Why Bedsores Happen in Nursing Homes
Neglect Isn’t Always Loud — Sometimes It’s Quiet and Deadly
When we speak with families across New Jersey, we often hear the same question: “How could this have happened?” The truth is, these injuries don’t usually stem from a single mistake—they develop over time due to a lack of basic care. In many cases, the cause is preventable. Below are the most common failures we see in long-term care facilities that result in serious harm. To explore similar issues related to negligent treatment, visit our page on nursing home neglect.
Poor Repositioning Practices
Routine repositioning is one of the simplest and most effective ways to protect immobile residents. It’s also one of the first responsibilities to fall through the cracks when a facility is understaffed. Without frequent turning—at least every two hours—blood flow is restricted and skin begins to deteriorate.
- Pressure builds on bony areas, like the tailbone or heels.
- Skin tissue breaks down, causing open wounds.
- Neglect of early symptoms means small problems become severe injuries.
In one instance, a resident was left in the same position overnight. By morning, they had developed a Stage 2 ulcer. Sadly, stories like this are not uncommon. For more information on how these injuries escalate, see our page on bedsores and pressure ulcers.
Staffing Shortages and Burnout
Many facilities in New Jersey operate under dangerous staffing conditions. When caregivers are stretched too thin, corners are inevitably cut—especially with vulnerable residents who require intensive attention. The impact of understaffing includes:
- Overwhelmed staff, unable to meet care standards.
- Inadequate monitoring, leading to missed signs of skin breakdown.
- Less training and supervision, especially with high turnover rates.
This isn’t just a staffing issue—it’s a systemic failure. Facilities are responsible for hiring and retaining enough qualified staff to meet residents’ needs. When they don’t, the consequences can be severe. We dive deeper into this issue in our section on nursing home negligence.
Lack of Individualized Care Plans
Not all residents are equally at risk. Those with diabetes, neuropathy, poor circulation, or mobility limitations need custom care plans. Sadly, many facilities take a one-size-fits-all approach, failing to conduct proper assessments or implement preventative measures.
We’ve reviewed cases where residents weren’t flagged as high-risk—despite clear medical histories. By the time family members noticed the damage, the wounds were already severe. This isn’t just a medical oversight; it’s a failure to treat patients as individuals. Learn how poor planning can lead to catastrophic outcomes by visiting our malnutrition and hydration care section, where similar gaps in individualized care are discussed.
Preventable Neglect vs. Unavoidable Conditions
Understanding What Nursing Homes Can — and Should — Control
One of the most common defenses we hear from nursing homes is that a resident’s bedsores were “unavoidable.” While it’s true that certain individuals face higher medical risks, this explanation often attempts to shift blame away from facility failures. In reality, most serious pressure ulcers develop because staff didn’t follow standard care protocols—not because of a resident’s health condition.
The Centers for Medicare & Medicaid Services (CMS) clearly states that a bedsore is only “unavoidable” if the facility has done everything medically necessary to prevent it. That means the care team must:
- Conduct and document detailed risk assessments
- Reposition residents regularly, typically every two hours
- Monitor and support proper hydration, nutrition, and hygiene
- Use pressure-relieving equipment like specialty mattresses and cushions
When these basic steps don’t happen—or when there’s no record of them—facilities cannot reasonably claim that the injury was beyond their control. In fact, we’ve worked on many cases where a nursing home tried to argue that a wound was inevitable, but the documentation showed missed turns, skipped monitoring, or complete gaps in care logs. If you want to see how we’ve held facilities accountable for these failures, visit our case results page.
What Courts and Experts Look For
When our team builds a bedsore case, we partner with independent doctors and wound care specialists to review the facts. These professionals examine whether staff followed proper medical protocols—and whether those actions aligned with state and federal standards. Courts often consider these critical questions:
- Did the care team develop a plan tailored to the resident’s needs?
- Were trained staff consistently implementing that plan?
- Did the facility monitor and update the care plan as the resident’s condition changed?
- Was there compliance with elder care regulations and industry standards?
When the answers reveal a pattern of neglect, families have strong grounds to pursue legal action. For example, if the care team skipped repositioning logs for multiple days, it shows a lack of attention and accountability. If you’re dealing with this situation now, we encourage you to learn more about your legal options by visiting our page on wrongful death and preventable injury claims.
Preventable Neglect vs. Unavoidable Conditions
Understanding What Nursing Homes Can — and Should — Control
One of the most common defenses we hear from nursing homes is that a resident’s bedsores were “unavoidable.” While it’s true that certain individuals face higher medical risks, this explanation often attempts to shift blame away from facility failures. In reality, most serious pressure ulcers develop because staff didn’t follow standard care protocols—not because of a resident’s health condition.
The Centers for Medicare & Medicaid Services (CMS) clearly states that a bedsore is only “unavoidable” if the facility has done everything medically necessary to prevent it. That means the care team must:
- Conduct and document detailed risk assessments
- Reposition residents regularly, typically every two hours
- Monitor and support proper hydration, nutrition, and hygiene
- Use pressure-relieving equipment like specialty mattresses and cushions
When these basic steps don’t happen—or when there’s no record of them—facilities cannot reasonably claim that the injury was beyond their control. In fact, we’ve worked on many cases where a nursing home tried to argue that a wound was inevitable, but the documentation showed missed turns, skipped monitoring, or complete gaps in care logs. If you want to see how we’ve held facilities accountable for these failures, visit our case results page.
What Courts and Experts Look For
When our team builds a bedsore case, we partner with independent doctors and wound care specialists to review the facts. These professionals examine whether staff followed proper medical protocols—and whether those actions aligned with state and federal standards. Courts often consider these critical questions:
- Did the care team develop a plan tailored to the resident’s needs?
- Were trained staff consistently implementing that plan?
- Did the facility monitor and update the care plan as the resident’s condition changed?
- Was there compliance with elder care regulations and industry standards?
When the answers reveal a pattern of neglect, families have strong grounds to pursue legal action. For example, if the care team skipped repositioning logs for multiple days, it shows a lack of attention and accountability. If you’re dealing with this situation now, we encourage you to learn more about your legal options by visiting our page on wrongful death and preventable injury claims.
When a Preventable Injury Becomes a Legal Matter
No family should have to wonder whether their loved one’s pain could have been avoided. Yet for far too many nursing home residents, bedsores are not just a medical issue—they are a warning sign of deeper, systemic neglect. These injuries cause real harm: physical suffering, emotional trauma, and often, life-threatening complications. And when they occur because of ignored protocols, understaffing, or carelessness, they are more than unfortunate—they are unacceptable.
At the Law Office of Andrew A. Ballerini, we believe in holding facilities accountable. With decades of experience in nursing home litigation, our team—including Certified Civil Trial Attorney Richard J. Talbot—knows what it takes to fight for justice. Whether the case involves untreated pressure ulcers, malnutrition, or a wrongful death, we approach every claim with compassion and trial-tested precision.
Let Us Help You Take the Next Step
If your loved one has suffered from pressure-related injuries in a nursing home, don’t wait for the facility to explain it away. Take action. Ask questions. Document everything. Then reach out to an advocate who understands the legal system and can guide you forward.
We offer free, confidential consultations and will meet with you at our office, in your home, or even at the hospital if needed. There are no upfront costs, and you don’t pay unless we recover compensation on your behalf.
To schedule your free consultation, contact our team today. We’re here to protect your loved one—and to make sure their pain leads to lasting accountability.